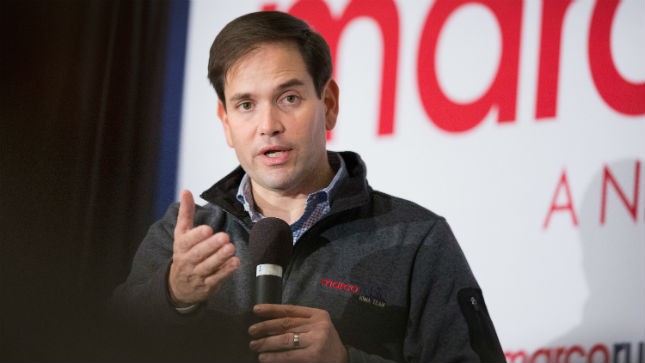
Sen. Marco Rubio may have dealt the biggest blow in the GOP’s five-year war against ObamaCare.
A 2014 budget measure inspired by the Florida senator and presidential hopeful is pushing some insurers to drop out of the ObamaCare exchanges, experts say.
“I think this is one of the most effective things they’ve done so far in terms of trying to undermine the Affordable Care Act,” Tim Jost, a healthcare law professor at Washington and Lee University, said of Republicans in Congress.
This fall, more than a dozen health insurers representing 800,000 people have dropped out of the ObamaCare exchanges, many out of fear that the administration no longer has the cash to cushion their losses in the costly early years of the marketplace.
The nation’s largest insurer, UnitedHealthCare, specifically mentioned the specter of a funding shortfall last week when it threatened to end its participation in the exchanges after 2016.
The angst in the industry centers on an obscure program in the healthcare law known as “risk corridors” that was designed to shield insurers against losses.
Rubio in 2013 went on the warpath against the program, decrying it as a “taxpayer bailout.” He penned op-eds against it, testified about it as the star witness at a House Oversight Committee hearing and even made his case to top House Republicans like then-Speaker John Boehner (R-Ohio).
“There is a problem with the way [ObamaCare] exchanges are now designed that have not yet received the attention they deserve, but I promise you’re going to be hearing a lot about it in the days to come,” Rubio said in a Senate floor speech in early 2014.
While Rubio’s attempt to scrap risk corridors altogether was unsuccessful, his push contributed to a policy rider that was inserted into a 1,603-page spending bill passed at the end of 2014.
Under the provision, which is still in effect, the Department of Health and Human Services (HHS) could no longer tap other accounts — like its overall appropriations or its Medicare funding — to fund the risk corridors program.
Now Rubio is taking his crusade against the "bailout" program to the presidential campaign trail.
The senator and dozens of other Republicans are seeking to renew the policy rider — or repeal risk corridors altogether — in the year-end budget bill that Congress must pass by Dec. 11 to avoid a government shutdown.
“So far, we’ve succeeded in stopping the Obama administration from bailing out healthcare companies under ObamaCare, and it’s critical that Congress once again stand with taxpayers to stop any taxpayer bailout of health insurers from happening,” Rubio wrote in a letter to GOP leaders of both chambers on Tuesday.
Defunding the program has also become a top issue for groups on the right.
On Tuesday, conservative groups such as Americans for Tax Reform and Heritage Action for America endorsed a letter to Speaker Paul Ryan (R-Wis.) and Senate Majority Leader Mitch McConnell (R-Ky.) urging them to keep the risk corridor restrictions in place.
Without them, the groups warned, the administration could have spent more than $2.5 billion of taxpayer money “to bailout insurers for their poor business decisions.”
“Taxpayers should not be on the hook for any more of Obamacare’s failures,” the letter said.
The risk corridors program was designed to be a temporary stopgap against high insurance claims during the first three years of the new federal program.
If an insurer had more expenses than it planned, the federal government would cover the remaining balance using cash collected from companies that paid out fewer claims than expected.
The program was almost certain to need extra money in the first few years, when there were fewer healthier customers signing up. But Rubio’s provision in 2014 severely limited any new spending by requiring the program to become budget neutral.
The damaging effects of the budget-neutral requirement became clear in October.
The Obama administration disclosed it could only afford to pay 13 cents of every dollar owed to the insurance companies — after insurers had already locked in their rates for the upcoming year.
“Obviously what happened was exactly what we thought would happen – there’d be an imbalance. Most of the companies lost money,” said Joseph Marinucci, a senior analyst with Standard & Poor.
“You have to be able to deal with unanticipated events, such as the legislation that would restrict the funding of its corridors,” he said.
Within weeks, about a dozen start-up insurers known as CO-OPs announced they’d be shutting their doors, in most cases because they lacked the cash flow to stay solvent. And at least two other insurers — WinHealth Partners in Wyoming and Moda Health in Washington — pulled out of the exchanges.
Then came the shocking announcement from the insurance giant, UnitedHealthCare, that it might cut its losses as well.
“Essentially what is happening now, and why you’re seeing all of these plans reevaluate their participation [in ObamaCare], they have to rely on their reserves over the next two years,” one industry source said. “It’s caused everyone to reevaluate and consider what changes they have to make to remain viable and stay in the market.”
The Obama administration has tried to reassure companies that it would “explore other sources of funding” — including working with Congress — in the case of another shortfall in 2016.
In her first public interview since UnitedHealth’s shareholder meeting, HHS Secretary pointed to companies like Aetna and Kaiser Permanente that are remaining “solidly in the marketplace” even after UnitedHealth’s announcement.
“We feel that, as we move forward, we have a product that the consumer wants and is satisfied with, and that it’s a place where issuers want to come and grow their business,” she said in an interview with Bloomberg TV.
But Jost, the healthcare professor, said big funding questions still lie ahead.
“Unless the administration does a really good job of negotiating the budget, I don’t see much can be done there,” he said. “Plans have known now for a number of years there wasn’t going to be new money for that program, but I think there still the hope that were would be more money from people paying into it.”
- Publish my comments...
- 0 Comments
